Exudative ARMD - Treatment Principles
Prior to the introduction of anti-VEGF drugs in 2006, the prognosis for patients with Exudative ARMD was not good. A small number of patients who were treated with thermal laser (prior to 2000) or PDT laser (after 2000) were lucky to have vision stabilized - better vision was not obtained. The majority of patients lost vision - just ask prior generations who had Exudative ARMD.
The inflection point of visual restoration occurred with the introduction of anti-VEGF drugs. Despite this success, the fact that the drug had to be injected into the vitreous or back part of the eye, proved to be a problem, ranging from a high level of treatment burden, i.e. multiple injections, as well as the risk for complications.
Here is the list of the anti-VEGF drugs that have been used since 2006:
- Macugen (first drug but no longer used)
- Avastin (most common drug used but not FDA approved for Exudative ARMD)
- Lucentis
- Eylea
- Beovu (infrequently used in the USA due to inflammatory complications)
- Vabysmo ( only drug that blocks both VEGF as well as Angiopoietin 2, another protein that stimulates abnormal blood vessel growth).
We use the term monotherapy to describe the use of one of these drugs at a time. We used the term combination therapy when more than one type of drug is used at the same time. More about this later.
The injections are given on a fixed frequency ( every 4 weeks) or a variable frequency ( as needed or treat and extend protocol where the time between injections is extended if the leakage remains stable). The original studies all included the use of every 4 week injections. Since then, we recognize that many patients do not need these drugs as often.
All the clinical studies have shown the safety and effectiveness of Lucentis, Eylea, Beovu, and Vabysmo. There is no proof that these drugs have specific risks unless a patient has had a heart attack or stroke within 6 weeks of the proposed injection. The injection, itself, has the most risk for injections, the worse been endophthalmitis, or infection in the eye, which can be quite serious and vision threatening. Thankfully, this only occurs infrequently. Recent advertisements for Vabysmo talk about elevated eye pressure after the injection. This occurs if the doctor does not drain the fluid out of the eye before or after an injection. Only 1% of doctors do this. Failure to do this does place the patient at risk for the development of glaucoma which can occur in up to 9% of patients.
Let's start with a few facts:
90% of patient who receive these drugs respond - i.e. resolution of neovascularization (abnormal vessels) and/or exudation (leakage) after the induction phase, i.e. two or three injections. If they do not, I call this a Primary AVF (Anti-VEGF Failure) - which comprises 10% of the patient population. Most doctors start treatment with a series of 2-3 monthly (fixed) injection (induction) and if they respond, the treatment frequency is decreased to a variable frequency. When this occurs, 30% of patients will start to leak again and/or the neovascularization might increase in size. This is called a Secondary AVF (Anti-VEGF Failure).
How does the doctor deal with this recurrent leakage which by all accounts represents a failure? Several choice are available:
- Change the anti-VEGF drug - this is not that easy as insurance often dictates which drugs can be used - your doctor will help with this change.
- Change the dosage of the anti-VEGF drug - this is now possible as Eylea is now available at a strength four times the standard dose (8 mg vs. 2 mg).
- Change the frequency of the anti-VEGF drug - if the doctor tried to extend your treatment from 4 to 8 weeks and if leakage recurs, the doctor can go back to 4 weeks again, i.e. inject you more frequently.
- Change the strategy with combination therapy, i.e. using different types of drugs to see if they work together better. Vabysmo is still considered a monotherapy however has two different proteins are being suppressed so by definition it is a combination therapy. Additionally, Photodynamic Therapy (PDT) can be combined with anti-VEGF therapy to create a true combination therapy. More on this later.
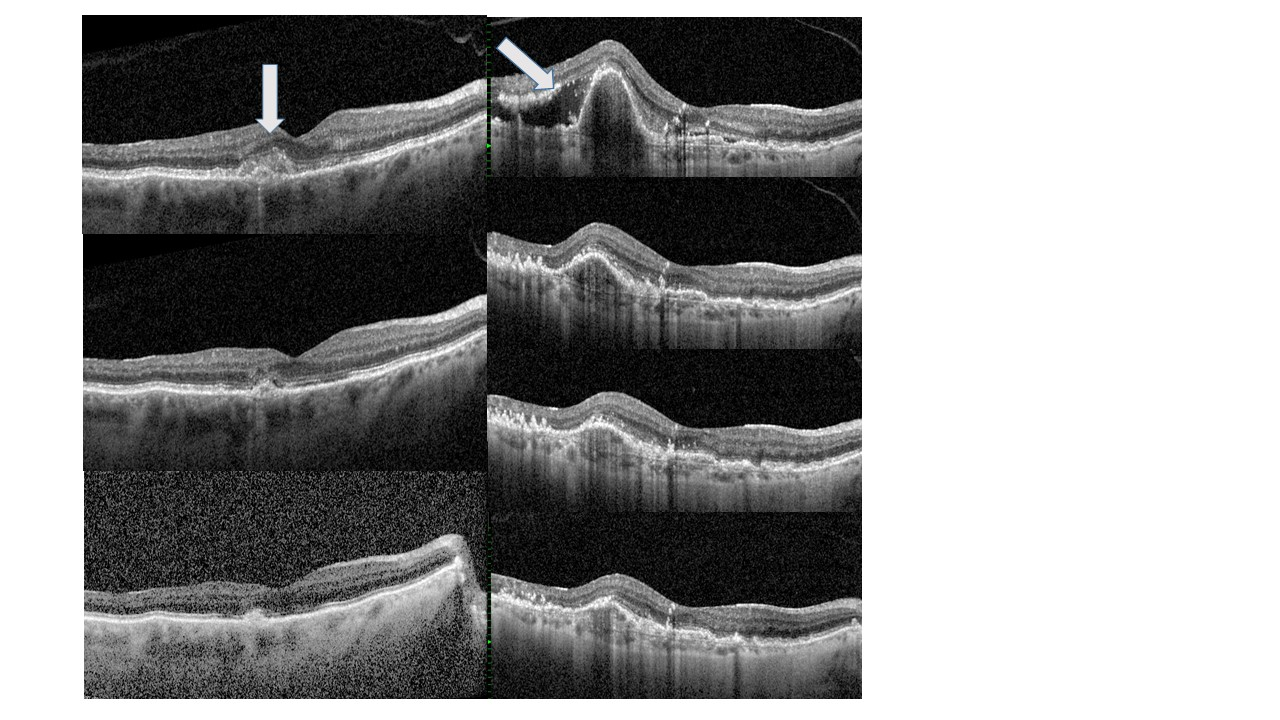
Let's start the discussion on how one can see if a drug works by giving an example - in the next blog post we'll talk more about the AVFs. In the photo below, the patient on the left has an early neovascularization - white arrow. These vessels regress or become smaller with subsequent injections (middle left and lower left). The same is true in the patient on the right. She has subretinal fluid (white arrow) and a retinal pigment epithelial detachment. Subsequent pictures shows the resolution of the subretinal fluid and the diminution of the RPE detachment.
Your doctor should be able to tell if the drug protocol is working or not working. Again, if the drug is not working, then one of the four steps above need to be entertained.